Happy Summertime! Here is an updated gluten-free grab and go list for everyone who is finally traveling, and an update on gluten and digestive research below. And I’m loving all the seasonal fruit!
Starting with the biggest news:
Labeling for gluten may be on the horizon! There’s a new bill that was introduced which would require companies to label gluten (not just wheat!) on all packages. This would be huge….contact your representatives! And many thanks to Gluten-free Watchdog for the alert.
Oh, the neat new Celiac studies! This one suggests that there may be a new pill to help with cross contamination on the way—or to enable people to eat gluten…note that the study is relatively small, and short length. And for those of you thinking that a pill is not for you, I respect that! There are people with Celiac eating a gluten-free diet whose numbers have not returned to normal who will likely be hugely helped by technology like this, and same goes for people who travel for work. Here’s the same research covered in NEJM
Speaking of travel, this new dining app from Gluten dude makes gluten-free dining out easier. Restaurants are either 100% GF or actually take good precautions.
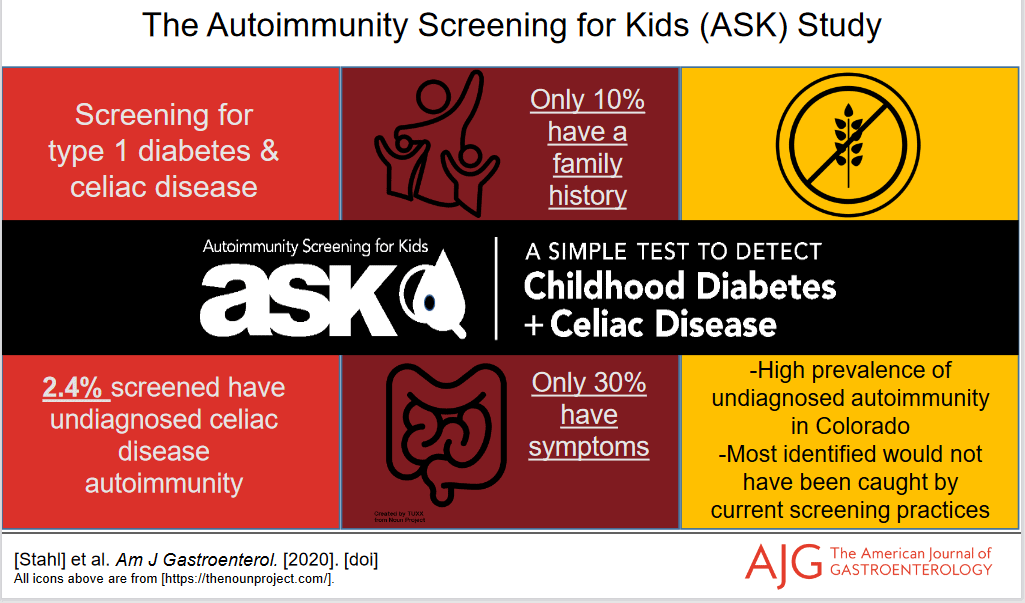
A study from the Center for Celiac Research suggests that there may be microbial changes before the development of Celiac—which hopefully may give new avenues for prevention down the line.
More about the microbiome in Celiac and RA
Ultra processed food is associated with risk of IBD–PURE study—this study links consumption of soft drinks, sweets, salty snacks, and processed meat with risk of UC and Crohn’s. Pros: it’s a big study, including people from different countries and regions, and it is a prospective study. Cons: correlation doesn’t mean causation. And nope, this still doesn’t mean the disease is your fault, but if you’ve got children at genetic risk, it’s something to consider. And as always, more study is needed.
This is a great overview of where the science is on the microbiome, which talks about everything from microbial diversity to busting many common myths.
For my fellow clinicians (or curious people) reading this, finally! IBS guidelines for pregnancy. All I can say is, it’s about time. Highlights—Low FODMAP should be adapted with an RD, soluble fiber is likely a plus, probiotics don’t have enough data.
A new randomized, controlled BMJ study shows that more dietary omega 3s may reduce migraines…
Enjoy the rest of your summer; it always goes by too fast!
Cheryl Harris, MPH, RD is a Registered Dietitian Nutritionist and Certified Wellcoach in Fairfax, VA. She helps people with a range of dietary issues, including Celiac Disease, digestive issues, preventing diseases and “whole foods” eating. Let’s get you on your way to achieving your goals and feeling great! Email or call 571-271-8742.

 The Farmers’ Market season has begun! Some, like Burke are open now, and I got asparagus, apples, sweet potatoes and a bunch of plants.
The Farmers’ Market season has begun! Some, like Burke are open now, and I got asparagus, apples, sweet potatoes and a bunch of plants. just put in potatoes, sweet potatoes, Thai peppers, basil and stevia, and more to come this weekend. I’ll put them in soon anyway and hope for the best. We also have a blackberry and blueberry plant, and even grapevines. The blackberry has a ton of flowers this year (right), which hopefully means there’s lots of fruit coming my way!
just put in potatoes, sweet potatoes, Thai peppers, basil and stevia, and more to come this weekend. I’ll put them in soon anyway and hope for the best. We also have a blackberry and blueberry plant, and even grapevines. The blackberry has a ton of flowers this year (right), which hopefully means there’s lots of fruit coming my way!



 Passover isn’t here until March 27th but many of the products are already appearing in grocery stores. Not all Passover foods are gluten-free, but many are, and there’s a much wider selection than usual at the grocery store. This can be a good time to stock up on GF cakes and mixes, cookies, macaroons, some of the “bread” crumbs and supplies like potato starch. As an added bonus for people with multiple restrictions, most Kosher for Passover products contain no corn or soy products, either.
Passover isn’t here until March 27th but many of the products are already appearing in grocery stores. Not all Passover foods are gluten-free, but many are, and there’s a much wider selection than usual at the grocery store. This can be a good time to stock up on GF cakes and mixes, cookies, macaroons, some of the “bread” crumbs and supplies like potato starch. As an added bonus for people with multiple restrictions, most Kosher for Passover products contain no corn or soy products, either.